By Laura Beavis and Loretta Lohberger
Posted Thu 2 Feb 2023 | Article Courtesy : https://www.abc.net.au
Emergency departments have become a ‘safety net’ — and we’re waiting in them longer than ever before
Melbourne mother Rachel Edmonds knows what it’s like to wait for hours in a hospital emergency department — both as a patient and as the mother of a sick toddler.
Her three-year-old son Austin needed hospital care several times during the height of the COVID-19 pandemic.
“In the waiting room he’d be screaming or crying, or, at times, lethargic,” she said.
“Unfortunately, the time we waited six hours was the time he was the sickest. They were particularly busy that time and they actually got him through quicker than the average wait time for that night.”
The experience was made more difficult by seeing other children in distress.
“It’s hard to switch off the empathy when you’re seeing all these other parents around you with their sick kids,” she said.
“Especially the new parents with the newborns and the young ones … you just wish you could help, but there’s nothing you can do because you’re in the same situation.”
Ms Edmonds said she had a complex medical history herself, which meant she often needed hospital care.
When she had gastro in September, Ms Edmonds said she went to the emergency department (ED) of her local public hospital where she waited 11 hours for a bed.
“I had collapsed on the floor about hour three, and I’d been told I wasn’t allowed to lie on the floor even though I was in quite a significant amount of pain and discomfort trying to sit in a chair because I was just so unwell.
“Generally, even when I’m not unwell, I can’t sit in a chair for a long period of time.”
Australians’ wait for treatment in EDs keeps getting longer
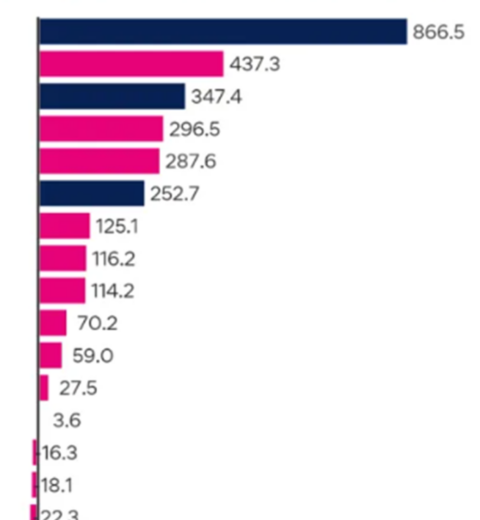
Data from the Productivity Commission reveals Ms Edmonds’s experience is not unique.
The annual Report on Government Services shows Australians are spending longer on average in EDs when they visit.
In 2021-22, only about 61 per cent of Australians left an ED within four hours, meaning 39 per cent were there for longer.
That was down from 67 per cent a year earlier, and 72.7 per cent in 2013-14.
The ACT had the lowest proportion of people leaving EDs within four hours last financial year, 52.4 per cent, down from 57 per cent a year earlier.
Tasmania was the second worst at 55.2 per cent, followed by Victoria with 55.3 per cent, South Australia with 57.6 per cent, and the Northern Territory with 58.8 per cent.
In Queensland 61.4 per cent of patients left EDs within four hours, it was 64.2 per cent in New South Wales and Western Australian was the best performer at 64.6 per cent.
All states and territories recorded a rise in waiting times last financial year compared with 2013-14.
More patients waiting longer than the national standard for treatment
The Productivity Commission also measured what proportion of people who went to EDs were treated within the national standard time frame, depending on how urgent their condition was.
Patients who required resuscitation were treated on time 100 per cent of the time in all hospitals except for South Australia and Tasmania, where the figure was 99 per cent.
For all triage categories, including emergency, urgent, semi-urgent, and non-urgent, the ACT was again the worst performer.
Only 48 per cent of patients were treated within the national benchmark waiting time in 2021-22, the same figure as a year earlier, but down from 61 per cent in 2013-14.
Western Australia was second worst at 50 per cent, followed by Tasmania (53 per cent), South Australia (55 per cent) and the Northern Territory (57 per cent).
In Victoria, the figure was 63 per cent, Queensland was 68 per cent, and New South Wales topped the table with 77 per cent of patients treated within the national benchmark waiting time.
Why are Australians waiting longer to get treatment in emergency departments?
Last financial year, there were nearly 8.8 million visits to Australian EDs, about 1.6 million more than a decade earlier.
Australasian College for Emergency Medicine president Clare Skinner said it was not only the number of presentations that were stretching EDs.
“We see people with complex care needs, people have multiple chronic illnesses, people are living much longer and there’s unfortunately also a much bigger burden of mental health in our communities,” Dr Skinner said.
People with complex healthcare needs take longer to treat, and often need to be admitted to hospital, but those hospital beds are increasingly unavailable.This situation is called bed block or access block: All of the acute beds in a hospital are full, so patients waiting in emergency department beds cannot be admitted.
“So everything gets slow and difficult, but then in turn that creates further blocks as [people] wait longer for access to the inpatient hospital services they require,” Dr Skinner said.
COVID-19 has exacerbated the pressure on EDs, but problems were developing before the pandemic.
Dr Skinner said Australia’s healthcare system was no longer fit for purpose.
“Emergency departments have become the safety net of the entire health and social services system, so when there are problems elsewhere in the system we’ll see people increasingly present to the emergency department,” she said.
“So we would really like to see the government take this critical opportunity to change our healthcare system so it matches the healthcare needs that Australians have today.”