Published 7 Aug 2023 By Olivia Willis and Margaret Burin | Article Courtesy : https://www.abc.net.au
The morning is peaceful. There are only three women in labour. But we are warned against using the Q word.
“Quiet.”
The midwives at Joan Kirner Women and Children’s at Sunshine Hospital in Melbourne’s west know just how quickly things can change.
It’s one of the busiest maternity services in Victoria; last week, 31 babies were born in 36 hours.
Taryn Madden is one of six women booked in for an induction today, but she’s been in labour since Wednesday morning.
Note: the following story contains images of childbirth.
It’s now Friday and her contractions are picking up.
Her midwife, Gemma, along with two student midwives, help her to change positions.
Taryn’s plan is to have a water birth with as little intervention as possible.
“You’re doing so well,” her partner Nathan reassures her.
But Taryn is exhausted.
“I can’t do this,” she says, begging to know how much longer it will take.
You’re already doing it, her midwives say, reminding her she is capable.
Gemma provides a comforting presence, guiding her through the pain and the unknown.
Taryn clutches the laughing gas, breathing hard and fast, as the midwives help her move into a warm bath.
They offer gentle encouragement and support, knowing there could be many more hours to come.
A few doors down, a midwife named Bailey is getting ready to deliver a baby for a first-time mum. It’s only Bailey’s fifth birth as a registered midwife.
The mum she’s caring for was induced yesterday and now is in the final stages of labour.
An epidural has brought her pain relief after 12 hours of intense contractions. She’s had an hour of rest, and now it’s time to push.
“You’re going to meet your baby on this next contraction,” Bailey says.
A few moments later, a baby boy enters the world and is quickly placed onto his mother’s chest.
A senior midwife gives the boy’s back a firm rub and a few seconds pass before a sharp cry pierces the room as the newborn takes his first breath of air.
The relief on his parents’ faces is visible.
After the newborn spends some time in his parents’ arms, Bailey gently places him on the scales and performs a quick physical check.
Soon, she will take the newborn and his mum upstairs to the maternity ward where they will be cared for and readied to go home.
By 1pm, there is a flurry of activity in the birthing unit staffroom.
A junior midwife updates her manager on the progress of a woman in labour, while another group of midwives arrive to start the afternoon shift.
“Can anyone do a double shift?” the unit manager asks.
For those who have just clocked on, it will mean working through until 7am.
It’s a question that will be familiar to midwives around the country.
In recent years, maternity services have been under significant pressure due to serious workforce shortages.
In some places, maternity units have been forced to close or reduce services, while others have struggled to keep up with demand.
The pandemic has also exacerbated many pressures that were starting to emerge before 2020, says Tanya Farrell, the director of maternity services at Western Health, which includes Joan Kirner.
“Like all services, we have had challenges in attracting midwives because the pool of midwives available to us lessened,” she says.
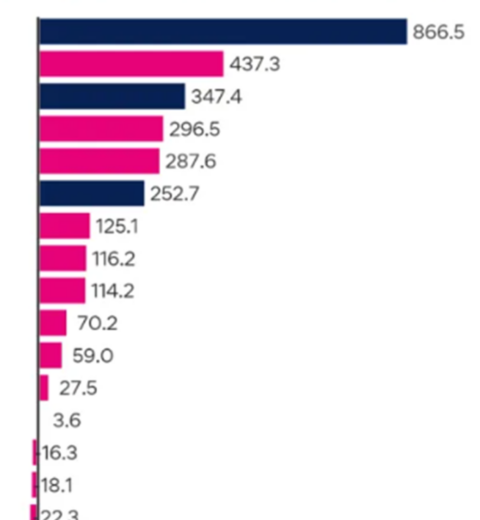
Nationally, the number of people working in midwifery declined by 1,220 between 2016 and 2022, health department data shows.
Meanwhile, a record 315,000 babies were born in 2021.
Last year, the National Skills Commission found there were midwife shortages in every state and territory.
A potential ‘catastrophe’
NSW Nurses and Midwives’ Association Assistant general secretary Michael Whaites says union members across Australia have reported “a shortage of experienced midwives on every shift”.
“Shifts are not being filled or they are being filled by people who are not midwives – either registered nurses or student midwives,” he says.
Heavy workloads are driving senior midwives to reduce their hours or leave the profession altogether, he says.
“What it means for the less experienced midwives is that they don’t have the support and the skills and knowledge around them on a daily basis.”
At one major Sydney hospital alone, there were 23 vacant midwife positions last month, the union estimates.
Some regional and rural services are so short-staffed they have as little as half the midwives they need – a problem compounded by doctor shortages in the regions, Mr Whaites says.
As well as forcing some women to travel further to access maternity services, he says staff shortages are compromising the quality of care.
“If you’re looking after more than one woman in active labour, how do you provide [a high] level of care?
“Midwives are having to make a decision about who’s getting their care at that moment and who’s not, and not knowing what’s in the room further down the corridor.
“That might be an inconvenience [for women and babies] – or it might be a catastrophe.”
In services that are understaffed, women are missing out on crucial support before and after birth, Australian College of Midwives chief midwife Alison Weatherstone says.
Adding to the challenge is that those accessing maternity services have increasingly complex needs. Today, women giving birth are, on average, older and more likely to be overweight.
While midwife-to-patient ratios vary from state to state, midwives working on postnatal wards are typically expected to care for up to six women – and their babies – overnight.
But Ms Weatherstone says not all states have ratios, and sometimes midwives are caring for even more.
“What happens is that midwives are just scrambling to provide the basic care and can’t spend time with women going through breastfeeding or providing postnatal education and support,” she says.
Data shows women and newborns are being discharged earlier now than in the past. This can mean less time surrounded by professionals while recovering from birth – and learning to care for their baby.
“If a woman has an experience that didn’t go to her plan or was a bit traumatic, then they’re not getting an opportunity to debrief and talk though that,” Ms Weatherstone says.
When midwives have ‘nothing left’
In 2021, a survey of more than 1,000 midwives in Victoria found almost three quarters were feeling burnt out and 40 per cent were regularly thinking about leaving the profession.
Lead researcher and clinical midwife Robyn Matthews says although midwives love the work they do, many find it difficult to provide high-quality care in strained, fragmented health systems.
“[Midwives] reported feeling really exhausted, that their workloads were incredibly heavy, that the number of women and babies that they were looking after wasn’t safe,” says Ms Matthews, who is completing a PhD at La Trobe University’s School of Nursing and Midwifery.
In some cases, she says midwives’ concern about the “over-medicalisation” of childbirth has added to their sense of “moral injury”.
“The more that you don’t get to do care the way that you want to, the more that affects you emotionally, and you become burnt out and you become cynical,” she says.
“And the worst thing in the world is a midwife who doesn’t care about the women she’s looking after because she’s got nothing left.”
As part of a crowd-sourced investigation into maternity care, the ABC heard from almost 450 midwives across the country.
Many of them told us understaffing was having serious impacts on patient care, and that at times, it felt unsafe.
“I work in a public hospital that is in crisis due to lack of staff … I regularly feel complicit in care that harms women.”
– Midwife in ACT
“I have often left my jobs feeling that I have completely failed women in one of the most vulnerable and pivotal times in their life. They’re alive at the end of the shift, but I have been unable to support them as they cried, bring them pain relief on time, do their vital observations … even change the blood-soaked sheets they’re sleeping in.”
– Midwife in regional NSW
“We force women to birth quickly because there are no staff to look after them on the night shift … And then in the postnatal period we kick them out before they know how to breastfeed because we have no beds and no staff.”
– Midwife in Perth
“It breaks my heart to imagine a woman I cared for writing to you, describing how neglected she felt on my ward under my care. The system failed us both. I work so bloody hard, and it’s not enough.”
– Midwife in Sydney
While data is limited, it’s estimated that as many as one in three Australian women experience birth trauma, which can be physical or psychological.
A Senate inquiry into birth trauma was recently announced in NSW after dozens of women complained about their treatment while giving birth.
Striving for ‘excellent care’
The Australian Health Practitioner Regulation Agency is currently conducting a Midwifery Workforce Review and is expected to deliver its recommendations to government in 2024.
Assistant Health Minister Ged Kearney says the federal government is looking at ways to attract and retain more midwifery staff, including streamlining the hiring process for overseas healthcare workers and removing barriers for midwives to practise privately.
“We need to make sure there is a robust workforce – that enough people are going into midwifery, that they can have fulfilling careers and work to their full scope of practice,” she says.
The government is also considering ways to encourage hospitals and maternity services to expand “continuity of care” models, she says, which involve women being looked after by the same midwives throughout their pregnancy, birth, and postpartum.
Research shows these models are associated with lower rates of medical intervention, as well as more positive experiences for mothers – and midwives.
In NSW, a spokesperson for the Department of Health says challenges in the midwifery workforce are being experienced in Australia and internationally.
“To ensure we continue to provide excellent care to our patients while recruitment progresses for vacant positions, we fill nursing and midwifery positions using current, casual and agency staff.”
The spokesperson says the NSW government is working with local health districts and universities to increase midwifery training positions and provide scholarships for rural postgraduate students.
Several state governments, including NSW and Victoria, have also pledged to introduce or improve midwife-to-patient ratios.
After a challenging few years, workforce pressures have eased at Joan Kirner with the return of healthcare workers from overseas, following the lifting of COVID-19 restrictions.
The hospital has also significantly increased the number of graduate midwives it accepts every year – from 20 to 70 – and introduced clinical educators to ensure its junior midwives are well supported.
Offering different models of care, including midwifery group practice and a home birth program, has also helped to attract and retain staff, maternity services director Tanya Farrell says.
“Our ultimate aim is to make sure that midwives can contribute to the work that they love for as many hours as they can,” she says.
“The challenge, however, is I still have to run a 24/7 service. Women need midwives to be here when the sun goes down.”
It’s just after midnight by the time Taryn finally gives birth to her daughter, Darci.
The birth hasn’t gone to plan, but Taryn says having the support of her midwives every step of the way “made it all better and less daunting”.
“They made everything so calm and secure – it didn’t matter that my whole birth plan went out the window,” she says.
“It’s a day that I’ll never forget.
“To bring her into the world, I don’t think anything will ever top it.”
Shortly after delivering Darci safely, Taryn’s midwife slips quietly out of the room.
The night is young, and more women will need her support.
Credits
- Reporting: Olivia Willis and Margaret Burin
- Photography: Margaret Burin
- Digital production and editing: Leonie Thorne
- Additional reporting: Kathleen Calderwood
This story is part of the ABC’s Birth Project