Posted Fri 22 Jul 2022 By Lucy MacDonald and Guy Stayner | Article Courtesy:https://www.abc.net.au
Australia is in the midst of a health crisis — one it cannot staff.
Key points:
- Unions say the country is facing a significant nursing shortage and things are only going to get worse
- The number of registered nurses in Australia has increased year on year, but the Australian Nursing and Midwifery Federation said there was still a severe shortage
- However, the ANMF cannot put a figure on the actual shortfall
More than two and a half years into the pandemic, COVID cases are once again on the rise.
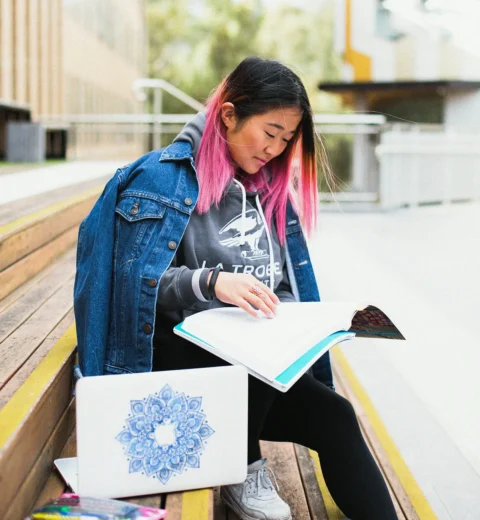
Nurses are needed more than ever, but they are burnt out and fatigued, and some are even leaving the industry.
Unions say the country is facing a significant nursing shortage and things are only going to get worse.
Royal Perth Hospital nurse Julie-Marie Hay has worked in the industry for 20 years, and said she was thinking about quitting because the pace was “relentless”.
“We’re constantly short of staff, we’re constantly asked to do more, we’re constantly asked to work more hours,” she said.
“Everybody is stretched, everybody is tired, we’re just absolutely exhausted.
“Morale is terrible. We’re not there for each other anymore. We can’t be, we don’t have time to be.
“We need more nurses, but we also need to retain more nurses,” she said.
The number of registered nurses in Australia has increased year on year — even during the pandemic.
But the Australian Nursing and Midwifery Federation (ANMF) said there was still a severe shortage.
“The number of vacant positions being advertised currently has doubled since this time last year,” said ANMF Federal Secretary Annie Butler.
“There’s at least 8,000 across the country, but we know that’s probably an underestimate.”
Most recent modelling from 2014
However, the ANMF cannot put a figure on the actual shortfall.
The most recent national modelling was done by Health Workforce Australia in 2014, shortly before it was decommissioned.
It predicted Australia’s demand for nurses would significantly exceed supply, with a projected shortfall of 85,000 nurses by 2025 or 123,000 by 2030.
“In the eight years since, there’s been absolutely no reasonable workforce planning, particularly not at a national level for our nursing and midwifery workforces,” Ms Butler said.
“So some of the things we could’ve been doing over the last eight years, we’ve just let go.
“So now a decade later, when we’re at this critical storm situation we’ve got to try and build back workforce planning, look at proper demand, supply studies, [and consider] what we need not just for the current situation, but what do we need into the future.”
Every state and territory needs nurses, and they are competing against each other.
Premiers have announced grandiose plans to create thousands of new healthcare jobs, but there has been little detail on where these new health workers will be recruited from and whether there will be enough to go around.
Victoria is offering international and returning Australian healthcare workers a $13,000 relocation allowance for those moving to regional areas and $10,000 for others with metropolitan jobs.
Queensland Health offers relocation packages for interstate and overseas candidates that include economy airfares for all dependents, furniture removal, temporary accommodation, visa and registration costs.
There are fears smaller states like Tasmania, which also offers its own relocation package, will be squeezed out of the market.
“At the moment, Tasmania is not competitive,” said Andrew Brakey from the Tasmanian branch of the ANMF.
“There are nurses who will go through a selection process, but at the end of that selection process when they work out their wages and the costs of living in Tasmania and their relocation costs, they’re deciding not to take up jobs they’ve been successful for.”
So how does Australia tackle the issue?
“[We need to make] sure that we try and offer similar incentives, make sure we are attracting nurses at an equal level across all states and territories,” said Ms Butler.
“Then we look at long-term measures to look at proper recruitment.”
Ms Butler said the union also encouraged “permanent migration” with close to 30 per cent of the workforce coming from a CALD background.
She said there were nurses “sitting offshore” who were ready and wanting to come. It was just a matter of speeding up the process.
“But if we bring nurses in from overseas, they have to be treated exactly the same way as Australian nurses … and we must abide by the parameters of ethical recruitment,” she said.
“We can’t just — to solve our own problems — seek to make the situation much worse in other countries.”
She also said limiting the spread of COVID and boosting primary care would take pressure off the system
“One of the easiest solutions is trying to get the community to assist us and support nurses … by trying to minimise the spread of COVID-19,” she said.
‘They are completely burnt out’
Taking pressure off the system is a big part of solving the crisis because states and territories do not just need to recruit nurses — they need to retain them.
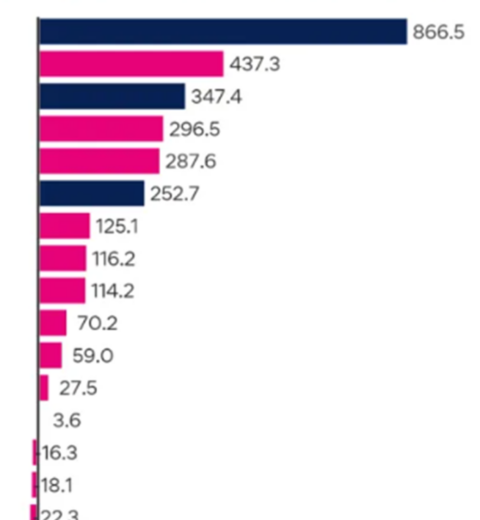
Federal data shows the number of nurses and midwives who are registered but not practising has increased by 63 per cent in the five years to 2021.
In Victoria, it has jumped by 85 per cent.
Those 8,000 vacancies mentioned earlier — the union says the majority are due to turnover, rather than new positions.
Ms Butler said the union was aware of nurses burning out and leaving the industry, while Victorian Branch Secretary Lisa Fitzpatrick said anecdotally: “The majority of our members are telling us they are reducing their shifts rather than leaving the professions.”
The union says the situation will worsen unless things improve for those already in the industry.
“They are completely burnt out and it’s very hard for them to see any light at the end of the tunnel,” said Ms Butler.
“When the situation just keeps intensifying and there is no respite, people are just going to say they’ve had enough and they’re going to leave and we do know that that is happening.”
‘We need to be shown that we are respected’
Perth nurse, Ms Hay understands.
“The last two years I’ve thought about quitting more than I ever expected I would ever consider quitting this industry. It’s absolutely heartbreaking,” she said.
But she has not quit, instead pouring her energy into fighting for better pay and conditions.
“It’s something that we enjoy because we care, but it’s hard work and it’s taking its toll on us now,” she said.
“We need to be shown that we are respected by giving us enough money to stay in the industry.”
State and territory governments responded by saying they have been successfully recruiting nurses and are continuing recruitment campaigns.
None provided a figure for the estimated shortfall.
The federal Department of Health said it had made clear commitments to boost the nursing workforce to ensure it continued to meet demand into the future.
It said for every nurse or midwife that exited the workforce via de-registration, 2.2 joined the workforce.
Finally, it said it was developing a national nursing workforce strategy to support the profession now and plan for the future.